Gastrointestinal
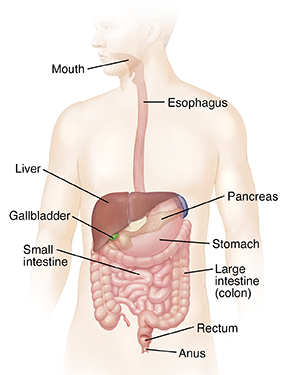
Anatomy of the digestive system
Food gives the body the energy needed for life. The digestive system breaks food down into basic nutrients that can be used by the body. The digestive tract is a long, muscular tube that extends from the mouth through the stomach and intestines to the anus. As food moves along the digestive tract, it's digested. This means it's changed into substances that can be absorbed into the bloodstream. Certain organs (such as the liver, gallbladder, and pancreas) help with this digestion. Parts of food that can't be digested are turned into stool. This is waste material that's passed out of the body.
Digestive system
The digestive system is made up of the following:
- The mouth. Takes in food, breaks it into pieces, and begins the digestion process.
- The esophagus. Moves food from the mouth to the stomach.
- Thestomach. Breaks food down into a liquid mixture.
- Theliver. Makes bile that helps digest fat, removes toxins from blood, and maintains healthy blood sugar levels.
- The gallbladder. Stores, concentrates, and controls the flow of bile into the small intestine.
- Thepancreas. Makes enzymes that help in digestion. And makes hormones that help control blood sugar.
- Thesmall intestine. Digests food further. And absorbs nutrients and water from food so they can be used by the body. What's left is passed on to the colon as liquid waste.
- The large intestine (colon). Absorbs water, salt, and minerals from the waste, forming a solid stool.
- The rectum. Stores stool until a bowel movement happens.
- Theanus. The opening where stool leaves the body.
Constipation
What is constipation?
Constipation occurs when your stools are painful. Or they don't happen often enough. It's the most common GI (gastrointestinal) problem.
You may have constipation if:
- You have bowel movements less than 3 times a week.
- Your stool is hard, dry, and in small pieces.
- You have to strain to have a bowel movement.
- It hurts to have a bowel movement.
Normal bowel movements vary depending on the person. They may happen as often as 3 times a day. Or they may happen just 3 times a week.
What causes constipation?
Your stool gets hard and dry when your colon (large intestine) absorbs (soaks up) too much water.
In most cases, as food moves through your colon, the colon absorbs water while it makes stool. Muscle movements (contractions) push the stool toward your rectum. When the stool gets to the rectum, most of the water has been soaked up. The stool is now solid.
If you have constipation, your colon's muscle movements are too slow. This makes the stool move through your colon too slowly. The colon absorbs too much water. The stool gets very hard and dry.
Some of the most common diet and lifestyle causes of constipation are:
- Not getting enough exercise.
- Not drinking enough liquids.
- Not eating enough fiber-rich foods.
- Not moving your bowels when you feel the urge to.
- Changes in your lifestyle, such as travel, pregnancy, and old age.
Other causes of constipation include:
- Medicines.
- A problem with how your stomach and bowels work (such as irritable bowel syndrome).
- Your intestine does not work well.
- Metabolic problems, such as thyroid disease.
- Intestinal blockage.
What are the symptoms of constipation?
Each person’s symptoms may vary. Symptoms of constipation may include:
- Difficult and painful bowel movements.
- Fewer than three bowel movements a week.
- Having a hard, dry stool that is hard to pass.
- Feeling bloated.
- Belly (abdominal) pain or discomfort.
- Straining to move your bowels without success.
Many of these symptoms may be caused by other health problems. Always talk with your health care provider to be sure.
How is constipation diagnosed?
Most people have constipation at one time or another. To see if you have constipation, your health care provider will do several tests. These tests will depend on how long you have had symptoms and how serious your case is.
First your provider will look at:
- Your age.
- If you have any blood in your stool.
- Any changes in your bowel habits.
- Weight loss.
Your provider will likely:
- Ask about your past health. You will be asked to give details about your constipation, such as how long you have had symptoms and how often you have bowel movements.
- Give you a physical exam. Your provider will do a full physical exam.
- Give you a digital rectal exam. This exam helps tell if the area is soft, blocked, or bloody. It can also check how much and what kind of stool you have. Your provider will also see if your rectum is bigger than normal. And they'll check the anal sphincters (muscles).
You may also need other tests, such as:
- Abdominal X-ray. This X-ray test can show if the bowels are full of stool (or air).
- Blood work. Blood is taken to make sure you don't have iron deficiency anemia, which may be a sign of slow bleeding from the colon.
- Lower GI series (also called barium enema). This is an X-ray exam of your rectum, the large intestine, and the lower part of your small intestine. You will be given a fluid called barium. It coats the organs, so that they can be seen on an X-ray. An X-ray of your belly will show if you have any narrowed areas, blockages, or other problems. An X-ray of the area around the anus and rectum (called a defecogram) may be done to see how well you can hold and release stool.
- Colonoscopy. This test looks at the full length of your large intestine. It can help check for any abnormal growths, tissue that is red or swollen, sores (ulcers), or bleeding.
- Sigmoidoscopy. This test lets your provider check the inside of part of your large intestine. It helps to tell what is causing constipation.
- Colorectal transit study. This test shows how long it takes for food to move through your colon. You will be asked to swallow pills (capsules) filled with small markers that can be seen on an X-ray. The X-rays will show how the capsules moved through your colon.
- Anus and rectum (anorectal) function tests. These tests can tell if you are constipated because your anus or rectum is not working well.
How is constipation treated?
Your health care provider will come up with a care plan for you based on:
- Your age, overall health, and past health.
- How serious your case is.
- How well you handle certain medicines, treatments, or therapies.
- If your condition is expected to get worse.
- Your opinion and what you want to do.
In most cases, diet and lifestyle changes can help reduce constipation symptoms. They can also stop it from happening. These changes may include:
- Drinking more water and juice.
- Getting regular exercise.
- Giving yourself time to have a bowel movement each day. Sitting for 10 minutes after meals can be helpful.
- Eating more fiber. If you don't eat enough fiber, add a fiber supplement.
- Taking laxatives. Your provider can discuss your choices.
- Stopping or changing medicine.
- Add a footstool in front of your toilet to raise your legs. This puts you in a better position to move your bowels.
- Doing physical therapy with or without biofeedback (part of a special physical therapy program).
| Foods | Moderate fiber | High fiber |
|---|---|---|
| Bread | Whole-wheat bread, granola bread, wheat bran muffins, grain bars, waffles, popcorn | |
| Cereal | 100% whole-grain cereals, oatmeal, granola, and oat bran | 100% bran cereals |
| Vegetables | Beets, broccoli, Brussels sprouts, cabbage, carrots, corn, green beans, green peas, acorn and butternut squash, spinach, potato with skin, avocado | |
| Fruits | Apples with peel, dates, papayas, mangoes, nectarines, oranges, pears, kiwis, strawberries, applesauce, raspberries, blackberries, raisins | Cooked prunes, dried figs |
| Meat substitutes | Peanut butter, nuts | Baked beans, black-eyed peas, garbanzo beans, lima beans, pinto beans, kidney beans, chili with beans, trail mix |
What are possible complications of constipation?
Constipation can cause other health problems, such as:
- Hemorrhoids. Red, swollen veins in the rectum. They happen when you need to keep straining to have a bowel movement.
- Anal fissures. Tears in the skin around the anus. They happen when hard stool stretches your sphincter muscle. They can cause bleeding in your rectum.
- Rectal prolapse. This is when a small amount of your intestinal lining pushes out from your anal opening. It is caused by straining to have a bowel movement.
- Fecal impaction. This is when a large lump of hard, dry stool stays stuck in your rectum. The colon’s normal pushing action can’t push out the stool. This is seen mostly in children and older adults.
Can constipation be prevented?
Many of the same lifestyle changes that help treat constipation may also help to stop it from happening:
- Have plenty of fiber, water, and liquids each day.
- Get daily regular exercise. Adults should do 150 minutes (2 hours and 30 minutes) of moderate intensity exercise every week. If you are new to exercise, this can be broken down into 10-minute periods of activity during the day. Daily movement activities, such as walking, gardening, house cleaning. count. They can make a big difference in how you feel.
- Allow plenty of time for bowel movements. When you feel the urge to have a bowel movement, be sure to do it.
- Try to have a bowel movement at the same time each day.
- If another health problem makes you more likely to have constipation, take your health care provider’s advice for treating that problem.
When to get medical advice
Most people have constipation at one time or another. But contact your health care provider if:
- Constipation lasts longer than 3 weeks.
- Constipation pain is stopping you from doing your daily activities.
- You have lasting pain in the rectum or belly.
- You have unexplained weight loss.
- You have symptoms of any of the complications of constipation.
- You have rectal bleeding, or see blood in the toilet bowl. It may be mixed in with the stool.
Key points about constipation
- Constipation is the most common GI (gastrointestinal) problem.
- You may be constipated when your stools are painful and happen less than 3 times a week.
- Your stool will be hard, dry, and in small pieces.
- Your stools get hard and dry when your colon absorbs too much water.
- Constipation symptoms can include stomach cramps and feeling tired.
- Constipation can cause other health problems, such as hemorrhoids (red, swollen veins in the rectum).
- Making diet and lifestyle changes can reduce constipation symptoms. These changes can also stop constipation from happening.
Next steps
Tips to help you get the most from a visit to your health care provider:
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions, especially after office hours or on weekends.
Description: Constipation is not being able to have bowel movements often enough. It can cause pain and other symptoms. Learn more about the causes, tests, and treatments for this common GI (gastrointestinal) problem. API URL: https://api.krames.com/v3/content/85-P00363
What is diarrhea?
Diarrhea is when your stools are loose and watery. You may also need to go to the bathroom more often. Diarrhea is a common problem. It may last 1 or 2 days and go away on its own. If it lasts more than 4 days, it may mean you have a more serious problem.
Diarrhea may be either:
Short-term (acute). This type lasts 1 or 2 days and then goes away. It may be caused by food or water that was made unsafe by bacteria. Or it may happen if you get sick from a virus or a food toxin.
Long-term (chronic). This type lasts several weeks. It may be caused by another health problem such as irritable bowel syndrome. It can also be caused by a digestive disease, such as Crohn’s disease, ulcerative colitis, exocrine pancreatic insufficiency, or celiac disease. Some infections, such as parasites, can cause chronic diarrhea.
What causes diarrhea?
Diarrhea may be caused by many things, including:
A bacterial infection.
A virus.
Food poisoning.
Trouble digesting certain things (food intolerance).
Food allergy, such as to milk.
Parasites that enter the body through food or water.
A reaction to medicines.
An intestinal disease, such as inflammatory bowel disease.
A problem with how your stomach and bowels work (functional bowel disorder), such as irritable bowel syndrome.
A result of surgery on the stomach or gallbladder.
Recent antibiotic use.
Metabolic problems such as thyroid conditions.
The pancreas not making enough enzymes to help digest food (exocrine pancreatic insufficiency).
Other less common reasons, such as damage from radiation treatments or tumors that make too many hormones.
Many people get traveler's diarrhea. This happens when you have food or water that is not safe because of bacteria, parasites, and food poisoning.
Severe diarrhea may mean you have a serious disease. See your doctor if your symptoms don’t go away or if they keep you from doing your daily activities. It may be hard to find out what is causing your diarrhea.
What are the symptoms linked with diarrhea?
Each person’s symptoms may vary. Symptoms associated with diarrhea may include:
Belly (abdominal) cramps.
Stomach pain.
Swelling (bloating).
Upset stomach (nausea or vomiting).
Urgent need to go to the bathroom.
Fever.
Bloody stools.
Loss of body fluids (dehydration).
Leaking stool and not being able to control your bowels (incontinence).
Dehydration is a serious side effect of diarrhea. Symptoms include:
Feeling thirsty.
Not urinating as often.
Having dry skin as well as a dry mouth and nostrils (mucous membranes).
Feeling very tired.
Feeling that you may pass out or faint (lightheaded).
Headaches.
Fast heart rate.
Diarrhea symptoms may look like other health problems. Bloody diarrhea is always a concern. Always see your doctor to be sure. Tell the doctor about any bleeding, fever, or vomiting.
How is diarrhea diagnosed?
To determine if there is a cause of diarrhea, your doctor will give you a physical exam and ask about your past health. You may also have lab tests to check your blood and urine.
Other tests may include:
Stool studies, including culture and other tests. This test checks for inflammation, digestion problems, or any abnormal bacteria or parasites in your digestive tract that may cause diarrhea and other problems. To do this test, a small stool sample is taken and sent to a lab.
Sigmoidoscopy. This test lets your doctor check the inside of part of your large intestine. It helps tell what is causing diarrhea. A short, flexible, lighted tube (sigmoidoscope) is put into your intestine through the rectum. This tube blows air into your intestine to make it swell. This makes it easier to see inside. A small tissue sample (biopsy) can be taken if needed.
Colonoscopy. This diagnostic procedure looks at the full length of your large intestine. It can help check for any abnormal growths, tissue that is red or swollen, sores (ulcers), or bleeding. A long, flexible, lighted tube (colonoscope) is put into your rectum up into the colon. This tube lets your doctor see the lining of your colon and take out a small tissue sample (biopsy) to test it. They can also treat some problems that may be found.
Imaging tests. These tests can see if there are any problems with the way your organs are formed (structural abnormalities).
Fasting tests and oral food challenges. These tests show if you are unable to digest certain foods (food intolerance). They can also tell if certain foods bring on an immune system reaction (food allergy).
Blood tests. These can look for metabolic problems like thyroid disease, anemia (low blood count), low vitamin levels that can mean poor absorption, and celiac disease, among other things.
How is diarrhea treated?
Treatment depends on your diagnosis. The severity of your symptoms, age, and general health may also impact treatment decisions.
In most cases, you will need to replace the fluids you have lost. If dehydration is severe, the best replacement is called an oral rehydration solution instead of fruit juice or sports drinks. You may also need a medicine that fights infection (antibiotic) if a bacterial infection is causing your diarrhea. Antidiarrheal medicines are commonly used. But they should not be used if you have bloody diarrhea or diarrhea with a fever.
What are possible complications of diarrhea?
If your diarrhea is severe, you are at risk for dehydration. Severe dehydration can lead to organ damage, shock, fainting (loss of consciousness) or coma, and even death.
What can you do to prevent diarrhea?
Having good personal habits can keep you from getting diarrhea caused by bacteria or a virus. They include:
Wash your hands often.
Use alcohol-based sanitizers.
Eat foods that have been cleaned and cooked in a safe way.
Don't eat or drink any foods or liquids that may have been infected with a bacteria or virus.
When you are traveling, check that anything you eat and drink is safe. This is even more important if you travel to developing countries.
Travel safety tips for water and other liquids include:
Not drinking tap water or using it to brush your teeth.
Not using ice made from tap water.
Not drinking milk or milk items that have not gone through a process to kill certain bacteria (pasteurization).
Travel safety tips for food include:
Don't eat any fresh or raw fruits and vegetables unless you wash and peel them yourself.
Make sure all meat and fish have been cooked to a safe minimum internal temperature.
Don't eat raw or rare-cooked meat or fish.
Don't eat food from street vendors or food trucks.
Living with diarrhea
In most cases, diarrhea is a short-term problem. It usually only lasts for a few days. Take plenty of liquids when you’re having a bout of diarrhea.
Some health problems can make diarrhea last longer or keep coming back. These include inflammatory bowel disease and irritable bowel syndrome. If another health problem is causing your diarrhea, follow your doctor’s advice for treating that problem.
When to contact your doctor
Contact your doctor or get medical care if you have:
Diarrhea more often.
A greater amount of diarrhea.
Symptoms of dehydration, including feeling thirsty, tired, or dizzy or having less urine or a dry mouth.
Bloody diarrhea or black and tarry stools or a fever, or if you are vomiting.
Key points about diarrhea
Diarrhea is when your stools are loose and watery.
You may also need to go to the bathroom more often.
Short-term (acute) diarrhea lasts 1 or 2 days.
Long-term (chronic) diarrhea may last several weeks.
Diarrhea symptoms may include belly cramps and an urgent need to go to the bathroom.
Loss of fluids (dehydration) is one of the more serious side effects.
Treatment usually involves replacing lost fluids and treating the cause if known.
You may need an antibiotic medicine if a bacterial infection is the cause.
Next steps
Tips to help you get the most from a visit to your doctor:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your doctor tells you.
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your doctor gives you.
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are and when they should be reported.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how to contact your doctor if you have questions, especially after office hours and on weekends and holidays.
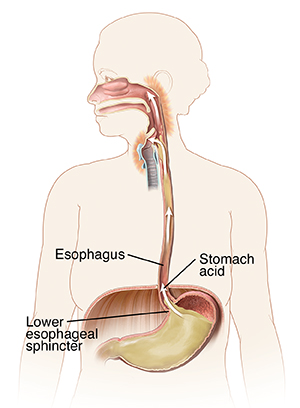
What Is GERD?
If you often have a painful, burning feeling in your chest after you eat, you may have gastroesophageal reflux disease (GERD). Heartburn that keeps coming back is a classic symptom of GERD. But you may have other symptoms as well. A GERD diagnosis is made only after a complete evaluation by your health care provider.
Important
Chest pain may also be caused by heart problems. Be sure to have all chest pain checked by a health care provider.
When you have a reflux problem
After you eat, food travels from your mouth down the esophagus to your stomach. Along the way, food passes through a one-way valve called the lower esophageal sphincter (LES). The LES sits at the opening to your stomach. Normally the LES opens when you swallow. It lets food enter the stomach, then closes quickly. With GERD, the LES doesn’t work normally. It lets food and stomach acid flow back (reflux) into the esophagus. This creates the burning sensation.
Some common symptoms
Common symptoms of GERD include:
- Frequent heartburn.
- Frequent burping.
- Sour- or acid-tasting fluid backing up into your mouth.
- Symptoms that get worse after you eat, bend over, or lie down.
- Trouble swallowing or pain when swallowing.
- A dry, long-term (chronic) cough, hoarseness.
- Upset stomach (nausea). Nausea and vomiting may be a sign of something else, so be sure to discuss with your health care provider.
Relieving your discomfort
You and your health care provider can work together to find the treatment choices to best ease your symptoms. These may include lifestyle changes, medicine, or possibly surgery.
Many people find their GERD symptoms decrease when they eat small frequent meals instead of 3 large ones. Reducing the amount of fatty, spicy, and acidic foods in your diet will also help.
Foods that tend to cause problems for people diagnosed with GERD include:
- Tomatoes and tomato products.
- Alcohol.
- Coffee.
- Peppermint.
- Greasy or spicy foods.
- Acidic foods, such as citrus.
To ease your symptoms, raise the head of your bed 4 to 6 inches. Don't eat anything within 2 to 3 hours of lying down.
If you are at a higher weight, losing weight will often ease GERD symptoms.
Stopping smoking may also help alleviate GERD symptoms.
Talk with your provider if you don’t understand how to make the dietary changes needed to control your GERD symptoms. Your provider can refer you to a nutritionist or recommend certain medicines to reduce the acid buildup.
What is an inguinal hernia?
An inguinal hernia is when part of your intestine pushes through a weak spot in your lower belly (abdominal) wall. This area is called the groin. The hernia creates a lump in your groin. Over time, the hernia may get bigger.
Most inguinal hernias, even large ones, can be made smaller and pushed back into your belly using gentle massage and pressure.
What causes an inguinal hernia?
There are two types of inguinal hernias: indirect and direct.
Indirect inguinal hernia. This is the most common type. It happens when an opening in your belly (abdominal) wall does not close normally before birth. That leaves a weak spot in the belly wall.
Direct inguinal hernia. This type occurs mainly in adult males. It is caused by a weakening of abdominal muscle tissue over time. This happens because of aging and long-term stress on the weakened belly muscles.
Who is at risk for an inguinal hernia?
An inguinal hernia can happen at any age.
You are at greater risk for an inguinal hernia if you:
Are male
Are obese
Are a pregnant woman
Have a family history of inguinal hernias
Smoke
Some activities may also raise your risk for an inguinal hernia. These include:
Doing a lot of heavy lifting
Long-term (chronic) coughing
Straining to have a bowel movement
What are the symptoms of an inguinal hernia?
Some inguinal hernias are painful while others don’t cause any pain.
Each person’s symptoms may vary. Symptoms may include:
A lump in the groin or in the sac that holds the testicles (the scrotum)
Pain or pressure in the groin that gets worse when you cough, strain, lift, or exercise
A burning feeling in the lump
Steady, growing pain if the blood supply to the bulging part of the intestine is cut off (called a strangulated hernia)
In severe cases, the intestine is partly or fully blocked. Symptoms in severe cases may also include:
Infection
Nausea
Vomiting
Lack of hunger
The symptoms of an inguinal hernia may look like other health problems. Always see your healthcare provider to be sure.
How is an inguinal hernia diagnosed?
Your healthcare provider will likely be able to tell that you have an inguinal hernia by looking at your past health and giving you a physical exam.
During the physical exam, they will try to push the hernia back into your belly.
You may also have imaging tests, including:
Ultrasound (sonography). This creates images of blood vessels, tissues, and organs on a computer screen using high-frequency sound waves. It is used to see the intestine and abdominal wall and check blood flow through different vessels.
X-ray. This test makes pictures of internal tissues, bones, and organs on large sheets of film. It uses invisible electromagnetic energy beams.
CT scan. This test shows detailed images of any part of the body, such as the bones, muscles, fat, and organs. A CT scan is more detailed than a regular X-ray. It uses a combination of X-rays and computer technology to make images of the body.
MRI. This test uses a magnetic field, radio waves, and a computer to view parts of the body.
How is an inguinal hernia treated?
An inguinal hernia will not heal on its own. If you have symptoms or the hernia is growing, you may need surgery.
There are two types of surgery for an inguinal hernia: traditional open hernia repair (herniorrhaphy) or laparoscopic hernia repair.
Open hernia repair. Your surgeon will cut the skin at the groin. They will push the bulging intestine back into your belly. Then, a stitch will close the opening in the muscle wall. Sometimes your surgeon may fix the weak area and make it stronger with mesh or wire (hernioplasty).
Laparoscopic hernia repair. Your surgeon will make a few small cuts (incisions) in your lower belly. They will insert a thin, flexible tube (laparoscope) into one of the cuts. The tube has a tiny video camera in it that is attached to a screen. This lets your healthcare provider see inside your belly. They will use long, thin tools in the other cuts to repair the hernia with mesh.
Inguinal hernias that are not causing any symptoms can be closely watched. If symptoms occur, your surgeon can repair the hernia through open surgery or laparoscopic surgery. Some surgeons recommend repair of all groin hernias in women. This is because it can be difficult to tell an inguinal hernia from a more complicated type of hernia (femoral hernia) in women.
You will need surgery right away if your small intestine gets stuck in the groin (incarcerated hernia) or if blood supply to your small intestine is blocked (strangulated hernia).
In some cases, a hernia may come back after surgery. This is less likely to happen when mesh is used to support the weak belly muscles.
What are possible complications of an inguinal hernia?
An inguinal hernia can lead to other problems such as:
Incarcerated hernia. This is when part of the small intestine gets stuck in the groin and can’t be pushed back into your belly. Get emergency medical care right away.
Strangulated hernia. If the incarcerated hernia is not treated, blood supply to the small intestine is blocked. This is a life-threatening condition. Get emergency medical care right away.
Hole (perforation). A hole (perforation) in the intestine may happen if the hernia is strangulated and part of the intestine dies from lack of blood. This is when the pinched-off part of the intestine, or bowel, is removed. In this case, you may need a bowel resection.
Peritonitis. If the hernia is sore and the skin over it is red and warm, you may have an infection of the lining of your belly (peritonitis).
Key points about inguinal hernia
An inguinal hernia happens when part of the intestine pushes through a weak spot in the belly (abdominal) wall.
The hernia creates a soft lump under the skin.
Most inguinal hernias can be pushed back into the belly with gentle massage and pressure.
An inguinal hernia will not heal on its own. If you have symptoms, or the hernia is growing, you may need surgery. Some surgeons recommend the repair of all groin hernias in women. Hernias that do not cause symptoms can be monitored, especially in men.
You will need surgery right away if your small intestine gets stuck in the groin (incarcerated hernia) or if blood supply to your small intestine is blocked (strangulated hernia).
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your healthcare provider tells you.
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your healthcare provider gives you.
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are and when you should report them.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your healthcare provider if you have questions.
Locations near you.
Recent News
News